Discover how cell biology research is revolutionizing cancer treatment, leading to more effective and personalized therapies. #CellBiology #CancerTreatment
How Cell Biology Research Drives Advances in Cancer Treatment
Table of Contents
“Unlocking the secrets of cells to conquer cancer – the power of cell biology research.”
Introduction
Cell biology research has been a crucial driving force behind the advancements in cancer treatment. The study of cells and their functions has provided valuable insights into the mechanisms of cancer development and progression. This has led to the development of new and more effective treatments that target specific cellular processes involved in cancer. In this introduction, we will explore how cell biology research has played a pivotal role in shaping the landscape of cancer treatment and improving patient outcomes.
The Role of Cell Signaling Pathways in Targeted Cancer Therapies
Cell biology research has played a crucial role in advancing our understanding of cancer and developing effective treatments. One area of cell biology that has particularly contributed to the development of targeted cancer therapies is the study of cell signaling pathways.
Cell signaling pathways are complex networks of molecules that allow cells to communicate with each other and respond to their environment. These pathways are involved in a wide range of cellular processes, including growth, division, and death. In cancer, these pathways can become dysregulated, leading to uncontrolled cell growth and tumor formation.
Targeted cancer therapies aim to specifically target and disrupt these dysregulated signaling pathways, while minimizing harm to healthy cells. This approach is in contrast to traditional chemotherapy, which often kills both cancerous and healthy cells, leading to severe side effects.
One of the most well-known examples of targeted cancer therapy is the use of tyrosine kinase inhibitors (TKIs) in the treatment of chronic myeloid leukemia (CML). CML is caused by a genetic mutation that leads to the overactivation of a signaling pathway called the BCR-ABL pathway. TKIs work by blocking the activity of the BCR-ABL protein, effectively shutting down the pathway and stopping the growth of cancer cells.
The development of TKIs was made possible by decades of research on cell signaling pathways. Scientists were able to identify the specific molecular targets within the BCR-ABL pathway and design drugs that could selectively inhibit them. This targeted approach has revolutionized the treatment of CML, with TKIs leading to high rates of remission and improved survival rates for patients.
In addition to TKIs, other targeted therapies have been developed based on our understanding of cell signaling pathways. For example, drugs that target the epidermal growth factor receptor (EGFR) have been successful in treating certain types of lung and colon cancers. EGFR is a key player in a signaling pathway that regulates cell growth and division. Mutations in the EGFR gene can lead to the overactivation of this pathway, contributing to the development and progression of cancer. By targeting EGFR with specific inhibitors, these drugs can effectively block the pathway and slow down the growth of cancer cells.
Another important aspect of cell signaling pathways in targeted cancer therapies is the concept of resistance. Cancer cells are notorious for their ability to develop resistance to treatments, rendering them ineffective over time. This is often due to mutations in the targeted pathway that allow cancer cells to bypass the effects of the drug. However, by understanding the mechanisms of resistance, scientists can develop new drugs or combination therapies that can overcome this resistance and improve treatment outcomes.
In addition to targeted therapies, cell signaling pathways have also played a role in the development of immunotherapies for cancer. Immunotherapies work by harnessing the power of the immune system to fight cancer. One type of immunotherapy, called checkpoint inhibitors, works by blocking the activity of proteins that prevent the immune system from attacking cancer cells. These proteins are often overexpressed in cancer cells, allowing them to evade detection by the immune system. By targeting these proteins, checkpoint inhibitors can unleash the immune system to attack and destroy cancer cells.
Cell signaling pathways are also involved in the development of cancer vaccines, which work by stimulating the immune system to recognize and attack cancer cells. By targeting specific signaling pathways involved in cancer growth and progression, these vaccines can train the immune system to recognize and destroy cancer cells.
In conclusion, cell biology research has been instrumental in driving advances in cancer treatment, particularly in the development of targeted therapies. By understanding the complex signaling pathways involved in cancer, scientists have been able to develop drugs and therapies that specifically target these pathways, leading to more effective and less harmful treatments for patients. As our understanding of cell signaling pathways continues to evolve, we can expect to see even more innovative and targeted approaches to treating cancer in the future.
Understanding Tumor Microenvironments: Implications for Immunotherapy
Cancer is a complex and devastating disease that affects millions of people worldwide. Despite significant advancements in cancer treatment, it remains one of the leading causes of death globally. However, recent developments in cell biology research have shed light on the intricate mechanisms of cancer growth and progression, leading to the development of new and effective treatments. One area of research that has shown promising results is the study of tumor microenvironments and its implications for immunotherapy.
Tumor microenvironment refers to the cellular and non-cellular components surrounding a tumor. These components include immune cells, blood vessels, and extracellular matrix, among others. The interactions between these components and cancer cells play a crucial role in tumor growth and progression. In the past, cancer treatment focused primarily on targeting cancer cells, but recent studies have shown that the tumor microenvironment also plays a significant role in cancer development and response to treatment.
One of the most promising treatments that have emerged from the study of tumor microenvironments is immunotherapy. This approach harnesses the power of the body’s immune system to fight cancer. The immune system is responsible for identifying and destroying abnormal cells, including cancer cells. However, cancer cells can evade the immune system’s detection by altering the tumor microenvironment. Understanding these interactions between cancer cells and the immune system is crucial in developing effective immunotherapies.
One of the key players in the tumor microenvironment is the immune cells. These cells, including T cells, B cells, and natural killer cells, are responsible for recognizing and eliminating cancer cells. However, in the tumor microenvironment, cancer cells can release signals that suppress the immune response, allowing them to grow and spread. Researchers have identified various mechanisms by which cancer cells evade the immune system, including the expression of immune checkpoint proteins and the recruitment of immune-suppressive cells.
The discovery of immune checkpoint proteins, such as PD-1 and CTLA-4, has revolutionized cancer treatment. These proteins act as brakes on the immune system, preventing it from attacking healthy cells. Cancer cells can exploit this mechanism by overexpressing these proteins, effectively shutting down the immune response. Immunotherapies targeting these proteins, known as checkpoint inhibitors, have shown remarkable success in treating various types of cancer, including melanoma, lung cancer, and bladder cancer.
Another crucial aspect of the tumor microenvironment is the extracellular matrix (ECM). The ECM is a network of proteins and other molecules that provide structural support to cells. In cancer, the ECM undergoes significant changes, leading to the formation of a dense and fibrotic environment. This dense ECM can act as a barrier, preventing immune cells from reaching the tumor. Additionally, the ECM can also release signals that suppress the immune response. Researchers are now exploring ways to target the ECM to improve the efficacy of immunotherapy.
Moreover, the tumor microenvironment also plays a role in the development of drug resistance. Cancer cells can adapt and evolve in response to treatment, making them resistant to traditional therapies. Recent studies have shown that the tumor microenvironment can contribute to this drug resistance. For example, the hypoxic conditions in the tumor microenvironment can promote the growth of cancer stem cells, which are known to be resistant to chemotherapy and radiation. Understanding these mechanisms can help researchers develop strategies to overcome drug resistance and improve treatment outcomes.
In conclusion, the study of tumor microenvironments has provided valuable insights into the complex interactions between cancer cells and their surroundings. This knowledge has led to the development of new and effective treatments, particularly in the field of immunotherapy. As research in this area continues to advance, we can hope for more breakthroughs in cancer treatment and ultimately improve the lives of those affected by this devastating disease.
Advances in Gene Editing Techniques for Precision Cancer Treatment
Cell biology research has been a driving force behind the advancements in cancer treatment. With a better understanding of the cellular mechanisms involved in cancer, scientists have been able to develop more targeted and effective treatments. One of the most promising areas of research in this field is gene editing techniques, which allow for precision treatment of cancer cells.
Gene editing techniques involve altering the genetic material of cells, either by adding, removing, or modifying specific genes. This can be done using various tools, such as CRISPR-Cas9, zinc finger nucleases, or TALENs. These techniques have revolutionized the field of cancer treatment, as they allow for precise targeting of cancer cells while minimizing damage to healthy cells.
One of the main challenges in cancer treatment is the ability to specifically target cancer cells without harming healthy cells. Traditional treatments, such as chemotherapy and radiation, can cause significant damage to healthy cells, leading to severe side effects for patients. Gene editing techniques offer a more targeted approach, as they can be designed to only affect cancer cells.
One of the most significant advantages of gene editing techniques is their ability to target specific mutations in cancer cells. Cancer is a complex disease, and different types of cancer can have different genetic mutations that drive their growth. By identifying these mutations, scientists can design gene editing techniques to specifically target and disrupt them, effectively stopping the growth of cancer cells.
Another advantage of gene editing techniques is their ability to enhance the body’s natural immune response to cancer. Our immune system is designed to recognize and eliminate abnormal cells, including cancer cells. However, cancer cells can evade the immune system’s detection by producing proteins that suppress the immune response. Gene editing techniques can be used to modify these proteins, making cancer cells more vulnerable to attack by the immune system.
One of the most promising applications of gene editing techniques in cancer treatment is CAR-T cell therapy. This approach involves extracting immune cells from a patient, modifying them using gene editing techniques to recognize and attack cancer cells, and then reintroducing them into the patient’s body. This personalized treatment has shown promising results in clinical trials, with some patients experiencing complete remission of their cancer.
In addition to targeting cancer cells directly, gene editing techniques can also be used to improve the effectiveness of traditional cancer treatments. For example, researchers have used gene editing techniques to modify cancer cells to make them more sensitive to chemotherapy drugs. This approach has shown promising results in preclinical studies and could potentially lead to more effective and less toxic treatments for cancer patients.
However, as with any new technology, there are still challenges and limitations to overcome in the use of gene editing techniques for cancer treatment. One of the main concerns is the potential for off-target effects, where the gene editing tools may unintentionally alter genes other than the intended target. This could lead to unintended consequences and potentially harmful side effects. Scientists are continuously working to improve the precision and safety of these techniques to minimize these risks.
In conclusion, gene editing techniques have opened up new possibilities for precision cancer treatment. By targeting specific mutations and enhancing the body’s natural immune response, these techniques offer a more targeted and effective approach to treating cancer. While there are still challenges to overcome, the potential for these techniques to revolutionize cancer treatment is promising. With continued research and advancements in this field, we can hope to see more personalized and effective treatments for cancer in the future.
Exploring the Potential of Stem Cells in Cancer Therapy
Cell biology research has been at the forefront of driving advances in cancer treatment. With the increasing prevalence of cancer and the limitations of traditional treatments, scientists have turned to exploring the potential of stem cells in cancer therapy. Stem cells, with their unique ability to self-renew and differentiate into different cell types, hold great promise in the fight against cancer.
One of the main challenges in cancer treatment is the ability of cancer cells to evade traditional therapies and continue to grow and spread. This is where stem cells come in. These cells have the ability to differentiate into different cell types, including cancer cells. By understanding the mechanisms behind this differentiation, scientists have been able to develop new treatments that specifically target cancer stem cells.
One such treatment is stem cell transplantation, also known as bone marrow transplantation. This procedure involves replacing damaged or diseased bone marrow with healthy stem cells. These stem cells then differentiate into healthy blood cells, providing a new immune system for the patient. This treatment has been particularly effective in treating blood cancers such as leukemia and lymphoma.
In addition to stem cell transplantation, researchers have also been exploring the potential of using stem cells to deliver targeted therapies directly to cancer cells. This approach involves engineering stem cells to produce and release anti-cancer drugs specifically at the site of the tumor. This not only reduces the side effects of traditional chemotherapy but also increases the effectiveness of the treatment by targeting only cancer cells.
Another promising area of research is the use of stem cells to regenerate damaged tissues and organs caused by cancer or its treatment. For example, breast cancer patients who undergo mastectomy often experience tissue damage and scarring. By using stem cells to regenerate healthy breast tissue, researchers hope to improve the quality of life for these patients.
Furthermore, stem cells have also been studied for their potential in immunotherapy, a type of cancer treatment that harnesses the power of the immune system to fight cancer. By using stem cells to produce immune cells that can specifically target and destroy cancer cells, researchers have been able to develop more effective and personalized immunotherapies.
However, despite the potential of stem cells in cancer therapy, there are still challenges that need to be addressed. One major concern is the risk of stem cells differentiating into cancer cells themselves. This is why extensive research is being conducted to understand the mechanisms behind stem cell differentiation and to ensure the safety of these treatments.
Moreover, the use of stem cells in cancer therapy is still in its early stages and more research is needed to fully understand their potential and limitations. This includes identifying the best sources of stem cells, optimizing their differentiation into specific cell types, and developing effective delivery methods.
In conclusion, cell biology research has been instrumental in driving advances in cancer treatment, particularly in the field of stem cell therapy. From stem cell transplantation to targeted drug delivery and tissue regeneration, the potential of stem cells in cancer therapy is vast. However, more research is needed to fully harness their potential and overcome the challenges associated with their use. With continued advancements in cell biology research, we can hope to see more effective and personalized treatments for cancer in the near future.
Q&A
1. How does cell biology research contribute to advancements in cancer treatment?
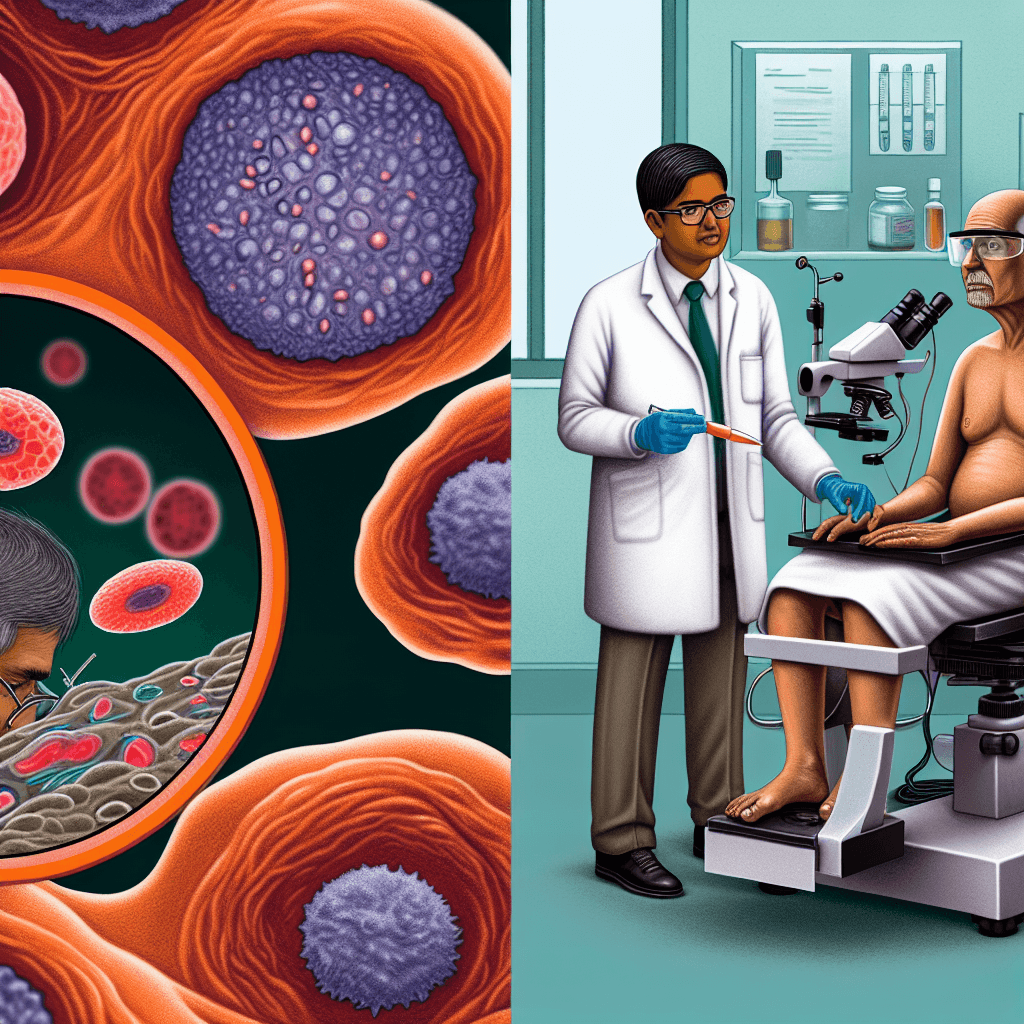
Cell biology research plays a crucial role in understanding the mechanisms of cancer development and progression. By studying the behavior and functions of cancer cells at a cellular level, researchers can identify potential targets for treatment and develop new therapies that specifically target cancer cells while minimizing harm to healthy cells.
2. What are some recent advancements in cancer treatment that have been driven by cell biology research?
Recent advancements in cancer treatment, such as targeted therapies and immunotherapies, have been made possible through cell biology research. Targeted therapies use drugs that specifically target certain molecules or pathways involved in cancer growth and progression, while immunotherapies harness the body’s own immune system to fight cancer cells.
3. How does understanding the biology of cancer cells help in developing more effective treatments?
Understanding the biology of cancer cells allows researchers to identify specific vulnerabilities and weaknesses that can be targeted with treatments. By studying the genetic and molecular changes that occur in cancer cells, researchers can develop more precise and effective treatments that can potentially improve patient outcomes and reduce side effects.
4. Can cell biology research also help in early detection and prevention of cancer?
Yes, cell biology research can also aid in early detection and prevention of cancer. By studying the cellular changes that occur during the development of cancer, researchers can identify biomarkers that can be used for early detection and develop strategies for cancer prevention. Additionally, understanding the underlying mechanisms of cancer can help in identifying risk factors and developing preventive measures.
Conclusion
In conclusion, cell biology research has played a crucial role in driving advances in cancer treatment. By understanding the complex mechanisms of cancer cells and their interactions with the body’s immune system, researchers have been able to develop targeted therapies and immunotherapies that specifically attack cancer cells while minimizing harm to healthy cells. Additionally, advancements in cell imaging and genetic sequencing have allowed for earlier detection and more personalized treatment plans for cancer patients. As cell biology research continues to evolve, it holds great potential for further advancements in cancer treatment and ultimately, improving patient outcomes.