Explore the Healthcare Claims Management Market: trends, size, share, and forecasts. Get key insights and data for strategic decisions.
Healthcare Claims Management Market Size, Share, Trends & Forecast

Table of Contents
Healthcare Claims Management Market Size, Share, Trends & Forecast

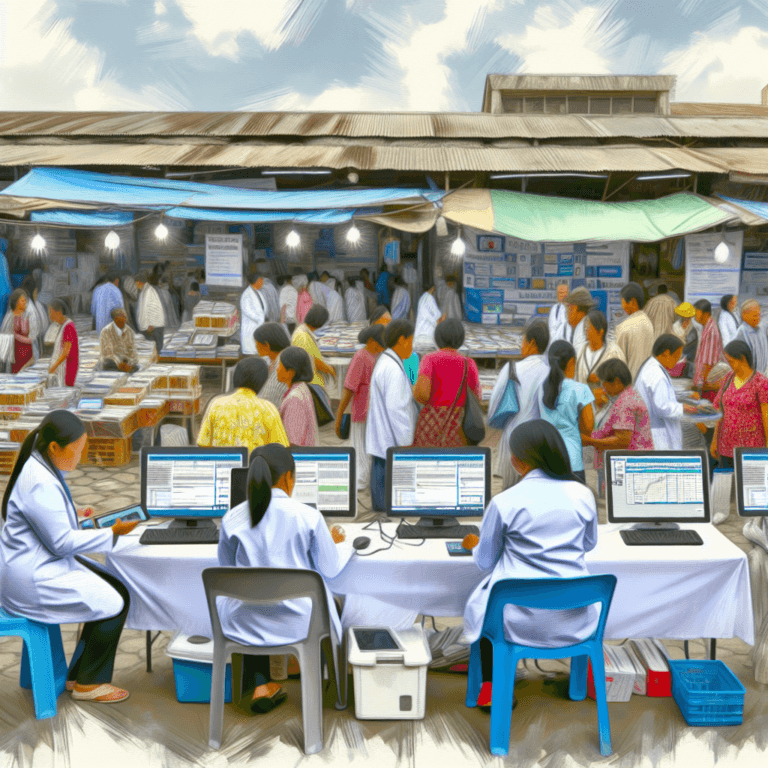
The healthcare claims management sector is a critical component of the healthcare industry, ensuring the smooth processing, billing, and management of health insurance claims. This market has seen significant growth due to the increasing demand for streamlined healthcare processes, advancements in technology, and the growing need for a reduction in healthcare costs. This article explores the current market size, shares, trends, and forecasts in healthcare claims management, providing insights into how these factors are shaping the industry.
Current Market Overview
The healthcare claims management market is currently witnessing robust growth. This growth is driven by several factors including technological advancements, regulatory changes, and an increase in the number of health insurance enrollees. The market encompasses various components such as software, services, and outsourcing solutions that help healthcare providers and insurers manage claims more efficiently.
Market Size and Forecast
According to recent studies, the global healthcare claims management market was valued at approximately USD 10.8 billion in 2020 and is expected to reach around USD 16.9 billion by 2028. This represents a compound annual growth rate (CAGR) of about 5.7% during the forecast period. The growth is primarily fueled by the increasing adoption of electronic health records (EHRs), government initiatives to update healthcare infrastructure, and rising healthcare expenditure.
Market Share and Regional Insights
The North American region holds the largest share of the healthcare claims management market. This dominance is attributed to the well-established healthcare infrastructure, high adoption rate of advanced technologies, and stringent regulatory standards regarding healthcare transactions. Following North America, Europe and the Asia-Pacific regions are also showing significant growth, the latter due to rapidly improving healthcare systems and increasing investments in healthcare IT solutions.
Key Trends Influencing the Market
- Integration of AI and Machine Learning: Artificial intelligence (AI) and machine learning are increasingly being integrated into healthcare claims management systems. These technologies help in automating the claims process, reducing errors, and improving the speed and accuracy of claims processing.
- Increasing Use of Cloud-Based Solutions: There is a growing trend towards cloud-based claims management solutions due to their scalability, flexibility, and cost-effectiveness. These systems also facilitate remote access to data, which is particularly beneficial in the context of the ongoing global shift towards remote work.
- Focus on Fraud Detection and Prevention: With the rise in healthcare fraud, there is an increasing demand for claims management solutions that incorporate advanced analytics to detect and prevent fraudulent activities.
- Regulatory Compliance: Healthcare providers are focusing more on compliance with regulations such as HIPAA in the U.S., which governs the privacy and security of certain health information. Compliance drives the adoption of updated claims management solutions.
Challenges in the Market
Despite the growth, the healthcare claims management market faces several challenges. These include the high cost of deploying claims management solutions and the lack of IT infrastructure in developing regions. Additionally, the complexity of claims management processes and the need for continuous updates in systems to keep up with changing regulations pose significant challenges.
Case Studies
Several case studies highlight the effectiveness of advanced claims management systems:
- Case Study 1: A major hospital in the United States implemented a new healthcare claims management system that integrates AI to predict and prevent claim denials. This system reduced their claim denial rates by 25%, significantly improving revenue flow.
- Case Study 2: An insurance company in Europe adopted a cloud-based claims management solution that enabled them to handle claims more efficiently and with greater transparency. This solution helped reduce processing times by 40% and improved customer satisfaction.
Future Outlook
The future of the healthcare claims management market looks promising with the integration of more advanced technologies like AI, machine learning, and blockchain. Blockchain, in particular, holds potential for enhancing the security and transparency of claims management. Furthermore, as global healthcare systems become more patient-centric, there is a growing emphasis on providing seamless claim processes, which will likely drive further innovations and developments in the market.
Conclusion
The healthcare claims management market is poised for significant growth, driven by technological advancements, regulatory changes, and an increasing need for efficient and cost-effective healthcare processes. While challenges such as high costs and complex regulations persist, the integration of new technologies and solutions are expected to overcome these hurdles, leading to improved healthcare outcomes and operational efficiencies. As the market continues to evolve, stakeholders in the healthcare industry must stay informed and adaptable to leverage the opportunities presented by these advancements.
In summary, the healthcare claims management market is a dynamic and essential facet of the global healthcare sector, crucial for the sustainability of healthcare systems worldwide. With continuous improvements and innovations, this market is expected to enhance the efficiency and effectiveness of healthcare services, benefiting providers, insurers, and patients alike.