“Learn how innovative solutions are bridging the gap in healthcare access and addressing disparities for all. Discover the future of equitable care.”
Addressing Disparities in Healthcare Access Through Innovation
Table of Contents
- Introduction
- Utilizing Telemedicine to Bridge the Gap in Rural Healthcare Access
- Innovative Solutions for Improving Healthcare Access in Underserved Communities
- Addressing Language Barriers in Healthcare through Technology and Cultural Competency Training
- Breaking Down Financial Barriers to Healthcare with Affordable and Accessible Options
- Q&A
- Conclusion
“Breaking barriers, bridging gaps – revolutionizing healthcare access for all.”
Introduction
Access to quality healthcare is a fundamental human right, yet disparities in healthcare access continue to persist globally. These disparities are often rooted in social, economic, and geographical factors, leading to unequal distribution of healthcare resources and services. However, with the rapid advancements in technology and innovation, there is a growing potential to address these disparities and improve healthcare access for all individuals. In this essay, we will explore the role of innovation in addressing healthcare disparities and its potential to create a more equitable healthcare system.
Utilizing Telemedicine to Bridge the Gap in Rural Healthcare Access
In today’s world, access to quality healthcare is a basic human right. However, for many individuals living in rural areas, this right is often not easily attainable. The lack of healthcare facilities and providers in these areas creates a significant disparity in healthcare access, leading to poorer health outcomes for rural populations. Fortunately, with the advancement of technology, there is a solution that can bridge this gap – telemedicine.
Telemedicine, also known as telehealth, is the use of technology to provide healthcare services remotely. It allows patients to connect with healthcare providers through video conferencing, remote monitoring, and other virtual communication tools. This innovative approach to healthcare delivery has the potential to revolutionize the way healthcare is accessed and delivered in rural areas.
One of the main challenges in rural healthcare is the shortage of healthcare providers. According to the Health Resources and Services Administration, there is a significant shortage of primary care physicians in rural areas, with only 11% of physicians practicing in these regions. This shortage makes it difficult for rural residents to access timely and quality healthcare services. However, with telemedicine, patients can connect with healthcare providers from anywhere, eliminating the need for physical proximity to a healthcare facility.
Moreover, telemedicine can also address the issue of transportation barriers in rural areas. Many rural residents live in remote areas, making it challenging to travel long distances to access healthcare services. This can be especially problematic for individuals with chronic conditions who require frequent medical appointments. Telemedicine allows patients to receive care from the comfort of their homes, reducing the need for transportation and the associated costs.
Another significant benefit of telemedicine is its potential to improve healthcare outcomes for rural populations. With the use of remote monitoring devices, healthcare providers can track patients’ vital signs and health data in real-time. This allows for early detection of health issues and timely intervention, leading to better health outcomes. Additionally, telemedicine can also provide access to specialists who may not be available in rural areas, allowing for more comprehensive and specialized care.
One of the most significant barriers to healthcare access in rural areas is the cost. Many rural residents are uninsured or underinsured, making it difficult for them to afford healthcare services. Telemedicine can help reduce these costs by eliminating the need for in-person visits, which can be expensive due to travel and accommodation expenses. Additionally, telemedicine can also reduce the cost of healthcare for patients by preventing unnecessary emergency room visits and hospitalizations.
However, despite its potential, there are still some challenges that need to be addressed for telemedicine to be fully utilized in rural areas. One of the main challenges is the lack of reliable internet connectivity in many rural regions. Without a stable internet connection, telemedicine services cannot be effectively delivered. This issue can be addressed through government initiatives to improve broadband infrastructure in rural areas.
Another challenge is the lack of awareness and acceptance of telemedicine among rural populations. Many individuals in these areas may not be familiar with this technology or may be hesitant to use it. Healthcare providers and organizations must educate and promote the benefits of telemedicine to increase its adoption in rural areas.
In conclusion, telemedicine has the potential to bridge the gap in healthcare access for rural populations. It can address the shortage of healthcare providers, transportation barriers, and high costs associated with accessing healthcare services in these areas. However, to fully utilize telemedicine, there is a need for investment in infrastructure and education to increase its adoption. With the right approach, telemedicine can be a game-changer in addressing healthcare disparities in rural areas and improving health outcomes for these underserved populations.
Innovative Solutions for Improving Healthcare Access in Underserved Communities

Access to quality healthcare is a fundamental human right, yet many individuals and communities around the world continue to face barriers in accessing essential healthcare services. These disparities in healthcare access are often more prevalent in underserved communities, where individuals may lack the resources and support needed to receive proper medical care. However, with the advancement of technology and innovative solutions, there is hope for addressing these disparities and improving healthcare access for all.
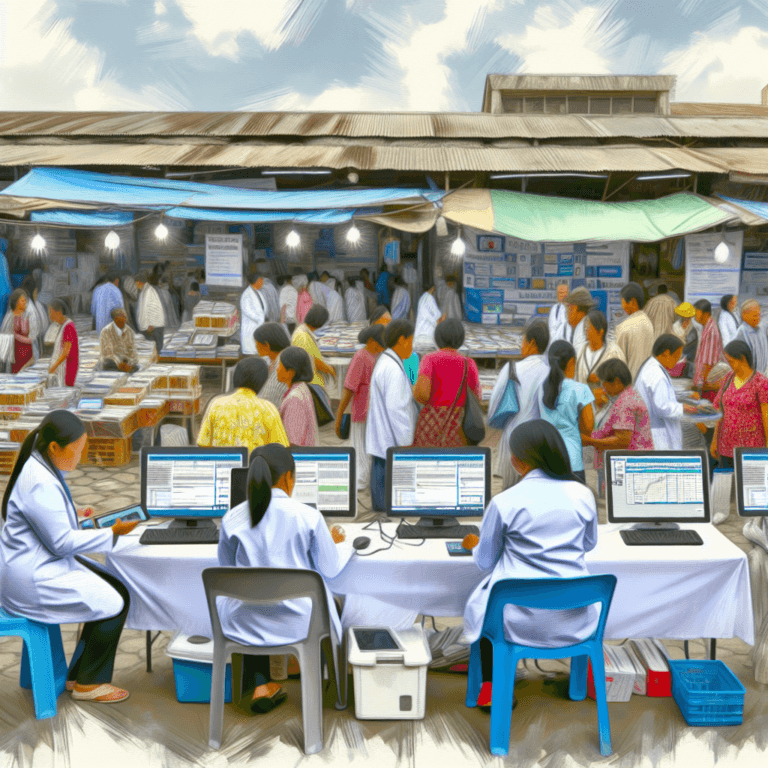
One of the main challenges in addressing healthcare disparities is the lack of access to healthcare facilities in underserved communities. Many individuals living in these areas may have to travel long distances to reach a hospital or clinic, making it difficult for them to receive timely and necessary care. This is where telemedicine comes in as a game-changing solution. Telemedicine, also known as telehealth, is the use of technology to provide remote healthcare services. It allows patients to connect with healthcare providers through virtual consultations, eliminating the need for physical travel.
Telemedicine has been particularly beneficial in rural and remote areas, where access to healthcare facilities is limited. With the use of telemedicine, patients can receive medical advice, diagnosis, and treatment from the comfort of their homes. This not only saves time and money but also ensures that individuals in underserved communities have access to quality healthcare services.
Another innovative solution for improving healthcare access in underserved communities is the use of mobile health clinics. These clinics are equipped with medical professionals and necessary equipment, and they travel to remote and underserved areas to provide healthcare services. Mobile health clinics have been successful in reaching individuals who may not have access to traditional healthcare facilities due to geographical or financial barriers.
In addition to physical barriers, financial constraints also play a significant role in healthcare disparities. Many individuals in underserved communities may not have health insurance or the financial means to pay for medical services. This is where community health workers (CHWs) have been instrumental in bridging the gap. CHWs are trained individuals from the community who provide basic healthcare services and education to their peers. They act as a liaison between the community and healthcare providers, helping individuals navigate the healthcare system and access the services they need.
Moreover, the use of electronic health records (EHRs) has also been a game-changer in improving healthcare access. EHRs are digital versions of patients’ medical records, which can be accessed and shared by healthcare providers. This eliminates the need for patients to carry physical copies of their medical records and allows for seamless communication between different healthcare facilities. EHRs have been particularly beneficial for individuals in underserved communities who may have to visit multiple healthcare providers for their medical needs.
Innovative solutions are not limited to technology and digital advancements. Community-based organizations (CBOs) have also played a crucial role in improving healthcare access in underserved communities. CBOs work closely with community members to identify their healthcare needs and provide tailored solutions. They also advocate for policy changes and work towards addressing social determinants of health, such as poverty and education, which can impact an individual’s access to healthcare.
In conclusion, addressing healthcare disparities in underserved communities requires a multifaceted approach. The use of technology, such as telemedicine and EHRs, has made significant strides in improving healthcare access. However, it is essential to also consider community-based solutions, such as mobile health clinics and CHWs, to ensure that all individuals have access to quality healthcare services. By combining these innovative solutions, we can work towards achieving equitable healthcare access for all.
Addressing Language Barriers in Healthcare through Technology and Cultural Competency Training
In today’s globalized world, healthcare providers are faced with the challenge of providing quality care to patients from diverse cultural and linguistic backgrounds. Language barriers can significantly impact the delivery of healthcare services, leading to disparities in access and quality of care. This is a pressing issue that needs to be addressed through innovation and cultural competency training.
One of the most effective ways to address language barriers in healthcare is through the use of technology. With the advancement of technology, there are now various tools and applications that can facilitate communication between healthcare providers and patients who speak different languages. For instance, telemedicine platforms allow for remote interpretation services, where a trained interpreter can assist in real-time communication between the patient and the healthcare provider. This not only improves the accuracy of communication but also ensures that patients receive the necessary care in a timely manner.
Another innovative solution is the use of translation devices. These devices can translate spoken words in real-time, making it easier for healthcare providers to communicate with patients who do not speak the same language. These devices are especially useful in emergency situations where time is of the essence. They also eliminate the need for a third-party interpreter, which can be costly and time-consuming.
In addition to technology, cultural competency training is crucial in addressing language barriers in healthcare. Cultural competency refers to the ability of healthcare providers to understand and effectively communicate with patients from diverse cultural backgrounds. This includes understanding their beliefs, values, and customs, which can impact their health and healthcare decisions.
Cultural competency training equips healthcare providers with the necessary skills to communicate effectively with patients who do not speak the same language. It also helps them understand the cultural nuances that may affect a patient’s perception of healthcare and their willingness to seek medical treatment. By promoting cultural competency, healthcare providers can build trust with their patients and provide more personalized care that meets their unique needs.
Moreover, cultural competency training can also help healthcare providers identify and address any biases or stereotypes they may hold towards patients from different cultures. This is crucial in providing equitable care to all patients, regardless of their background. By understanding and respecting cultural differences, healthcare providers can create a more inclusive and welcoming environment for their patients.
In addition to addressing language barriers, cultural competency training can also improve health outcomes for patients from diverse backgrounds. Studies have shown that patients who receive care from culturally competent providers are more likely to adhere to treatment plans and have better health outcomes. This is because they feel understood and respected, which can positively impact their overall satisfaction with the healthcare experience.
In conclusion, addressing language barriers in healthcare through technology and cultural competency training is crucial in promoting equitable access to quality care. By utilizing innovative solutions such as telemedicine platforms and translation devices, healthcare providers can bridge the communication gap with patients who speak different languages. Additionally, cultural competency training can help healthcare providers understand and respect the cultural differences of their patients, leading to improved health outcomes and a more inclusive healthcare system. It is essential for healthcare providers to embrace these strategies and continue to innovate in order to provide the best possible care for all patients, regardless of their cultural or linguistic background.
Breaking Down Financial Barriers to Healthcare with Affordable and Accessible Options
In today’s world, access to quality healthcare is a basic human right. However, for many individuals and communities, this right remains out of reach due to financial barriers. The high cost of healthcare services, coupled with limited insurance coverage, has created a significant disparity in healthcare access. This disparity is especially prevalent in low-income and marginalized communities, where individuals often have to choose between seeking medical treatment and meeting their basic needs.
To address this issue, innovative solutions are needed to break down financial barriers and make healthcare more affordable and accessible for all. In recent years, there has been a growing focus on developing such solutions, with the aim of bridging the gap in healthcare access and improving overall health outcomes.
One of the most promising innovations in this area is the use of telemedicine. Telemedicine involves the use of technology to provide remote medical services, such as consultations, diagnoses, and treatment. This approach has the potential to significantly reduce healthcare costs, as it eliminates the need for patients to travel to a physical healthcare facility. It also allows for more efficient use of healthcare resources, as doctors can see more patients in a shorter amount of time.
Another innovative solution is the use of community health workers (CHWs). CHWs are trained individuals who work within their own communities to provide basic healthcare services, such as health education, preventive care, and referrals to medical professionals. By bringing healthcare services directly to the community, CHWs can help reduce the financial burden on individuals who may not have the means to travel to a healthcare facility. They also play a crucial role in addressing cultural and language barriers that may prevent individuals from seeking medical care.
In addition to these solutions, there has been a growing trend towards the development of affordable and accessible healthcare options. This includes the use of generic drugs, which are significantly cheaper than brand-name drugs but have the same active ingredients and effectiveness. Generic drugs have been proven to be just as safe and effective as their brand-name counterparts, making them a viable option for individuals who cannot afford expensive medications.
Furthermore, the rise of retail clinics has also contributed to making healthcare more affordable and accessible. Retail clinics are walk-in medical facilities located in retail stores, pharmacies, and supermarkets. They offer basic healthcare services, such as vaccinations, screenings, and treatment for minor illnesses, at a lower cost than traditional healthcare facilities. This option is particularly beneficial for individuals who do not have health insurance or have high deductibles.
Innovative payment models have also emerged to address financial barriers to healthcare. One such model is value-based care, which focuses on paying healthcare providers based on the quality of care they provide, rather than the quantity of services. This approach incentivizes healthcare providers to focus on preventive care and improving health outcomes, rather than just treating illnesses. As a result, it can lead to cost savings for patients and improve overall healthcare access.
Finally, the use of technology has also played a significant role in making healthcare more affordable and accessible. Mobile health (mHealth) applications, for example, allow individuals to access healthcare services and information through their smartphones. These apps can provide remote consultations, medication reminders, and health tracking, making it easier for individuals to manage their health and access medical care.
In conclusion, addressing disparities in healthcare access requires innovative solutions that break down financial barriers and make healthcare more affordable and accessible. From telemedicine and community health workers to affordable options and innovative payment models, there are various approaches that can help bridge the gap in healthcare access. By embracing these innovations, we can work towards a future where quality healthcare is accessible to all, regardless of their financial status.
Q&A
1. What are some examples of healthcare disparities that exist today?
Some examples of healthcare disparities include unequal access to quality healthcare services based on race, ethnicity, socioeconomic status, geographic location, and insurance coverage. These disparities can lead to differences in health outcomes and treatment options for individuals from marginalized communities.
2. How can innovation help address healthcare disparities?
Innovation can help address healthcare disparities by creating new and improved methods of delivering healthcare services, such as telemedicine and mobile health clinics. It can also help improve access to healthcare by developing new technologies and tools that make healthcare more affordable and accessible for marginalized communities.
3. What role do government policies play in addressing healthcare disparities?
Government policies play a crucial role in addressing healthcare disparities by implementing laws and regulations that promote equal access to healthcare for all individuals. This can include policies that address insurance coverage, funding for healthcare programs, and addressing social determinants of health.
4. What are some potential challenges in addressing healthcare disparities through innovation?
Some potential challenges in addressing healthcare disparities through innovation include the cost of implementing new technologies and services, ensuring equal access to these innovations for all communities, and addressing any biases or inequalities in the development and implementation of these innovations. Additionally, there may be resistance to change from traditional healthcare systems and providers.
Conclusion
In conclusion, addressing disparities in healthcare access through innovation is crucial in ensuring that all individuals have equal opportunities to receive quality healthcare services. By utilizing technology and innovative solutions, we can bridge the gap between underserved communities and healthcare resources. This can lead to improved health outcomes and a more equitable healthcare system. It is important for healthcare organizations and policymakers to prioritize and invest in innovative approaches to address disparities and promote health equity for all individuals. Only through collaborative efforts and a commitment to innovation can we truly achieve equitable access to healthcare for all.