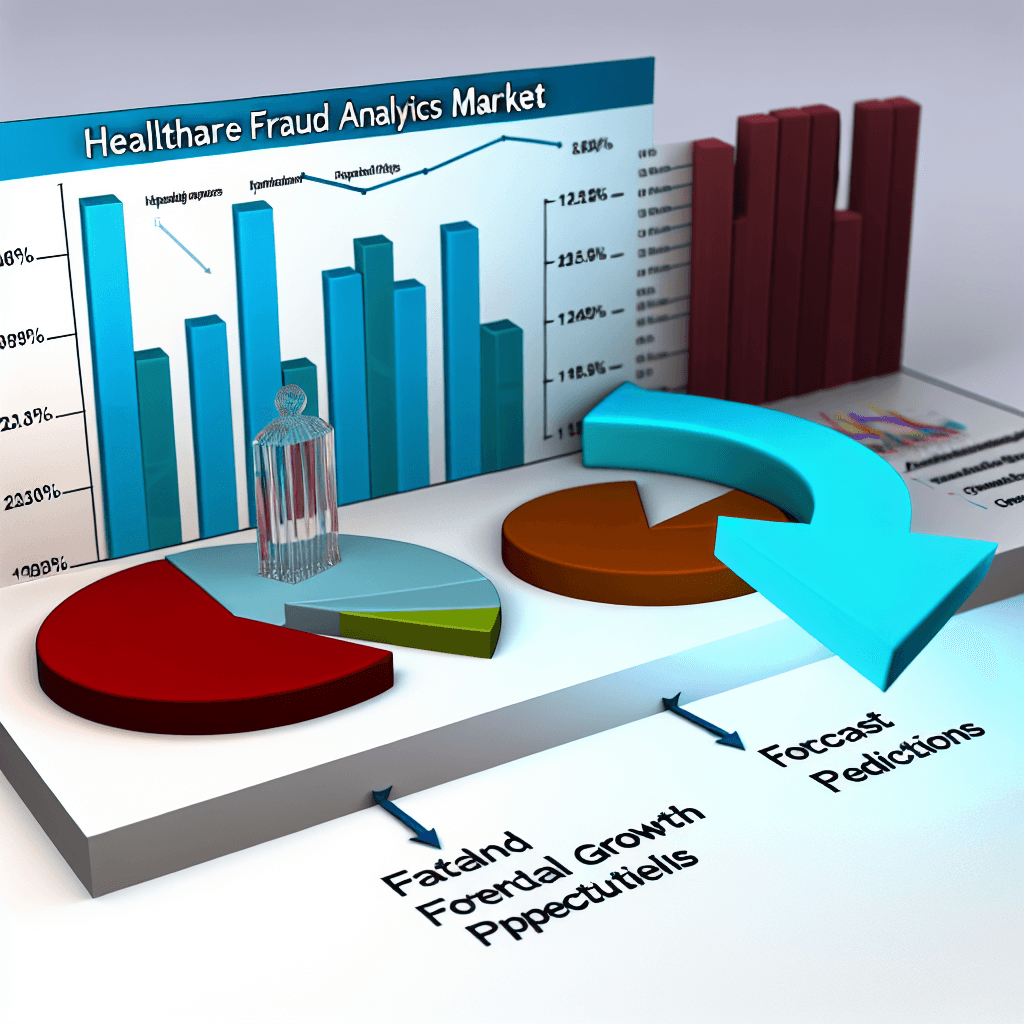
Explore the Healthcare Fraud Analytics Market size, share, opportunities, and forecasts. Unlock insights and trends for strategic decisions.
Healthcare Fraud Analytics Market Size, Share, Opportunities & Forecast
Table of Contents
Healthcare Fraud Analytics Market Size, Share, Opportunities & Forecast
The healthcare industry, while essential for societal well-being, is not immune to the challenges of fraudulent activities. Healthcare fraud involves the intentional deception or misrepresentation that the individual or entity makes, knowing that the misrepresentation could result in some unauthorized benefit to the individual, or other parties. In recent years, the rise in such activities has led to the increased adoption of healthcare fraud analytics. This article delves into the market size, share, opportunities, and forecasts of healthcare fraud analytics, providing a comprehensive overview of the landscape.
Understanding Healthcare Fraud Analytics
Healthcare fraud analytics refers to the use of data analytical tools and methods to detect and prevent fraudulent activities in healthcare settings. These tools analyze patterns and anomalies in the billing and claims data, helping organizations identify potentially fraudulent activities before they result in significant financial losses.
Market Size and Growth Drivers
The global healthcare fraud analytics market has witnessed significant growth over the past few years. According to a report by Grand View Research, the market size was valued at USD 1.2 billion in 2020 and is expected to grow at a compound annual growth rate (CAGR) of 27.7% from 2021 to 2028. This growth is driven by several factors:
- Increasing Number of Fraudulent Activities: As healthcare costs rise, so does the incentive for committing fraud. This has led to an increased demand for effective fraud detection and prevention solutions.
- Government Initiatives: Governments worldwide are implementing strict regulations and penalties for healthcare fraud, which compels healthcare providers to adopt advanced analytics solutions.
- Technological Advancements: Advances in machine learning, artificial intelligence, and big data analytics have enhanced the effectiveness of fraud detection tools, making them more attractive to healthcare providers.
- Rising Healthcare Expenditure: As global healthcare expenditure increases, the financial impact of fraud becomes more significant, driving investment in fraud prevention tools.
Market Segmentation
The healthcare fraud analytics market can be segmented based on several criteria:
- Type of Solution: Descriptive analytics, predictive analytics, and prescriptive analytics.
- Delivery Model: On-premise and cloud-based solutions.
- Application: Insurance claims review, pharmacy billing misuse, payment integrity, and others.
- End User: Public & government agencies, private insurance payers, third-party service providers, and others.
Each segment offers unique growth opportunities and challenges, influenced by technological, regulatory, and economic factors.
Regional Insights
The North American region holds the largest share of the healthcare fraud analytics market. This dominance is attributed to the well-established healthcare infrastructure, high healthcare spending, and stringent regulatory framework for fraud prevention. However, Asia-Pacific is expected to witness the highest growth rate due to increasing healthcare fraud, rising awareness about fraud analytics solutions, and growing healthcare infrastructure in countries like China and India.
Key Players and Competitive Landscape
The healthcare fraud analytics market is highly competitive with several global and regional players. Key players include IBM Corporation, Optum, Inc., SAS Institute, Inc., and McKesson Corporation. These companies are continually innovating and investing in research and development to stay ahead of the competition. For instance, Optum has developed advanced algorithms that can detect anomalies and patterns in real-time, significantly reducing the potential for fraud.
Case Studies and Success Stories
Several organizations have successfully implemented healthcare fraud analytics to combat fraud. For example:
- Medicare Fraud Strike Force: In the United States, the Medicare Fraud Strike Force uses advanced analytics to identify unusual billing patterns and has recovered billions of dollars in improperly paid claims.
- Private Insurance Company: A leading private insurance company implemented predictive analytics to detect fraudulent claims, resulting in a 40% reduction in suspect claims.
Future Opportunities and Market Forecast
Looking ahead, the healthcare fraud analytics market is poised for further growth. Opportunities lie in the integration of AI and machine learning technologies, which can enhance the predictive capabilities of fraud detection systems. Additionally, as more data becomes available and systems become more interconnected, the effectiveness of analytics tools will likely improve, leading to broader adoption.
Forecasts suggest that by 2028, the market could reach a valuation of approximately USD 4.6 billion, driven by continued technological advancements and increased global healthcare spending.
Conclusion
The healthcare fraud analytics market is a critical component in the fight against healthcare fraud. With substantial market growth, driven by technological advancements and increasing fraud instances, the adoption of these tools is becoming indispensable in modern healthcare settings. As the market continues to evolve, healthcare providers and payers must stay informed and consider integrating advanced analytics into their fraud prevention strategies to safeguard resources and enhance the efficiency of healthcare delivery.
In conclusion, the healthcare fraud analytics market not only offers robust solutions for combating fraud but also presents significant growth opportunities for technology providers. The future looks promising, with advancements in AI and machine learning poised to take fraud detection to new heights.