Explore the latest trends and forecasts in the Healthcare Provider Network Management Market, driving efficiency and connectivity in healthcare.
Healthcare Provider Network Management Market
Table of Contents
- Exploring the Healthcare Provider Network Management Market
- Understanding Healthcare Provider Network Management
- Key Components of Network Management
- Market Drivers and Trends
- Regulatory Compliance
- Technological Advancements
- Cost Containment Pressures
- Challenges in the Market
- Data Integration Issues
- Provider Resistance
- Complex Regulatory Environment
- Case Studies and Examples
- Case Study: A Large Health Insurance Company
- Example: Use of AI in Network Management
- Future Outlook
- Conclusion
Exploring the Healthcare Provider Network Management Market
The healthcare provider network management market is a critical component of the healthcare industry, focusing on improving the efficiency and effectiveness of healthcare delivery. This market involves a range of activities, from network design and provider contracting to management and compliance monitoring. As healthcare systems worldwide strive to enhance patient care while controlling costs, the role of network management has become increasingly important. This article delves into the various aspects of the healthcare provider network management market, exploring its importance, current trends, challenges, and future outlook.
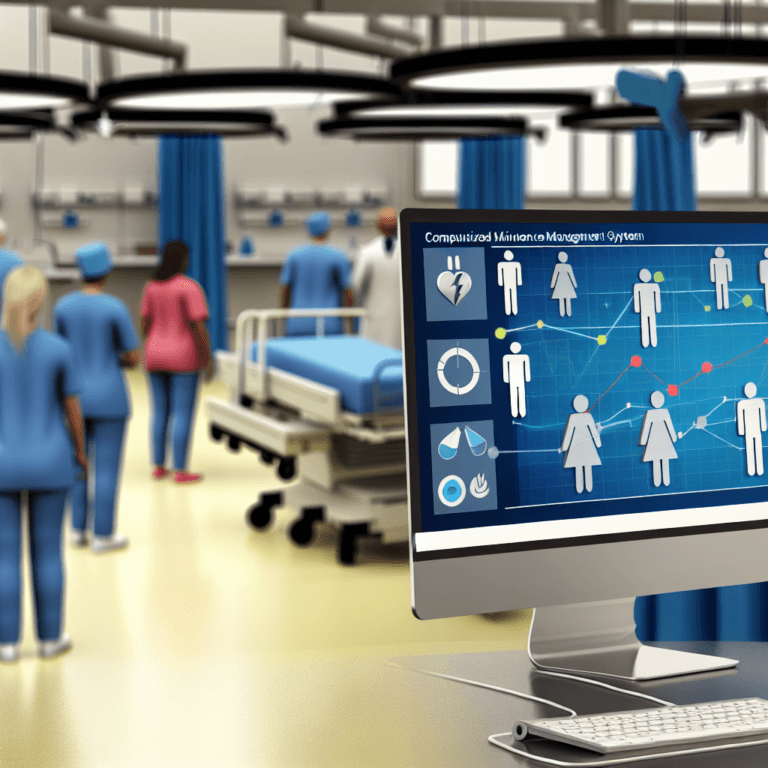
Understanding Healthcare Provider Network Management
Healthcare provider network management involves the administrative and operational tasks needed to handle healthcare provider networks effectively. These networks are composed of the doctors, hospitals, and other healthcare providers that a health plan contracts with to deliver medical services to its members. Effective network management ensures that patients have access to quality healthcare services while helping to control costs and maintain compliance with regulatory standards.
Key Components of Network Management
- Provider Credentialing
- Contract Management
- Performance Monitoring
- Compliance and Quality Assurance
- Payment Systems and Billing
Market Drivers and Trends
The healthcare provider network management market is driven by several factors that influence its growth and evolution. Understanding these drivers is essential for stakeholders to navigate the market effectively.
Regulatory Compliance
Increasing regulatory requirements around healthcare transparency and patient data protection are pushing healthcare organizations to adopt sophisticated network management solutions. For instance, regulations such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States mandate the protection of patient information, influencing how networks manage data.
Technological Advancements
Technological innovations, including the integration of AI and machine learning, are revolutionizing how networks are managed. These technologies help in predictive analytics, risk management, and efficiency enhancements in provider network operations.
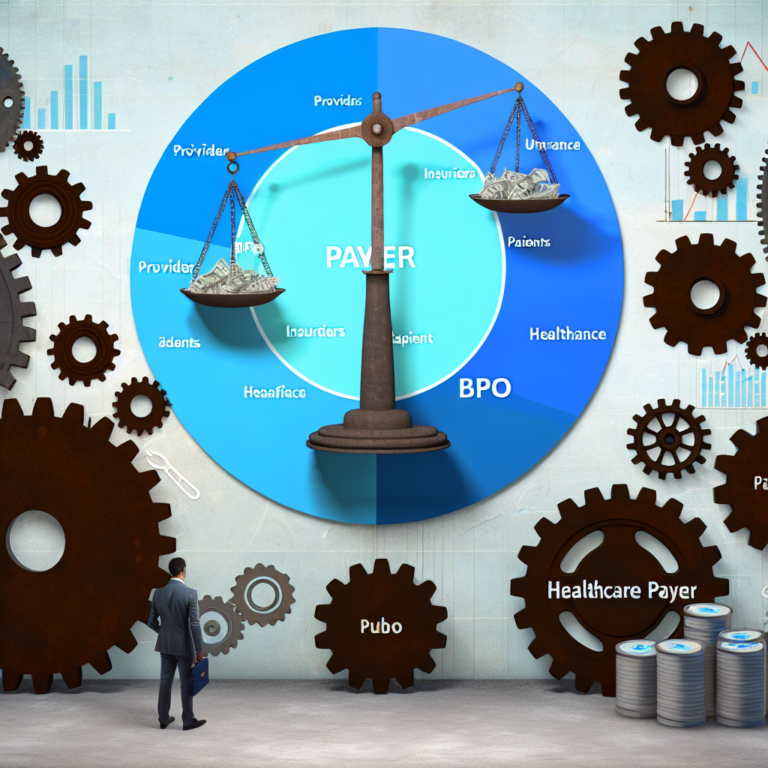
Cost Containment Pressures
As healthcare costs continue to rise, payers and providers are looking for ways to reduce expenses without compromising on quality. Effective network management helps in identifying cost-saving opportunities through optimized provider contracts and fraud prevention.
Challenges in the Market
Despite the growth, the healthcare provider network management market faces several challenges that could impede its progress.
Data Integration Issues
Integrating data from diverse sources and ensuring its accuracy and consistency remains a significant challenge. This integration is crucial for effective decision-making and operational efficiency.
Provider Resistance
Some healthcare providers are resistant to network management practices, particularly those that seem to prioritize cost over care. This resistance can hinder the implementation of effective management strategies.
Complex Regulatory Environment
Navigating the complex and often changing regulatory environment can be difficult, requiring continuous updates and adaptations in network management practices.
Case Studies and Examples
Several successful implementations of network management solutions provide insights into the practical benefits of effective network management.
Case Study: A Large Health Insurance Company
A major health insurance company in the United States implemented a comprehensive provider network management system that included advanced analytics and provider performance monitoring. This system allowed the company to enhance its network efficiency, reduce costs by 15%, and improve patient satisfaction scores.
Example: Use of AI in Network Management
An innovative startup developed an AI-powered tool that helps healthcare networks predict which providers might cause billing anomalies or suboptimal patient outcomes. This tool has been adopted by several healthcare networks, leading to improved compliance and patient care quality.
Future Outlook
The future of the healthcare provider network management market looks promising, with continued advancements in technology and an increasing focus on cost efficiency and quality care. The integration of AI and machine learning is expected to play a pivotal role in shaping the market, making network management more predictive and proactive.
Conclusion
The healthcare provider network management market is a vital aspect of the healthcare industry, essential for maintaining the balance between cost control and quality care. While the market faces challenges such as data integration difficulties and regulatory complexities, the advancements in technology and strategic innovations are likely to drive its growth. Stakeholders in the healthcare sector must stay informed and adaptable to leverage the opportunities presented by this dynamic market.
By understanding the components, drivers, and challenges of the healthcare provider network management market, healthcare organizations can better prepare themselves to meet the demands of an evolving healthcare landscape, ultimately leading to improved patient outcomes and operational efficiencies.