Discover the latest advancements in diagnostic testing technologies, from rapid results to increased accuracy, revolutionizing healthcare.
Key Innovations in Diagnostic Testing Technologies

Table of Contents
- Introduction
- Advancements in Point-of-Care Testing: How Rapid Results are Revolutionizing Diagnosis
- The Role of Artificial Intelligence in Diagnostic Testing: Enhancing Accuracy and Efficiency
- Next-Generation Sequencing: Unlocking the Potential of Genetic Testing for Disease Diagnosis
- Microfluidic Technology: Miniaturizing Diagnostic Testing for Improved Accessibility and Affordability
- Q&A
- Conclusion
“Revolutionizing healthcare, one test at a time with cutting-edge diagnostic technologies.”
Introduction
Diagnostic testing technologies have revolutionized the field of medicine, allowing for faster and more accurate diagnoses of various diseases and conditions. These innovations have greatly improved patient outcomes and have become an essential tool for healthcare professionals. In recent years, there have been significant advancements in diagnostic testing technologies, leading to more efficient and precise methods of detecting and monitoring diseases. In this article, we will explore some of the key innovations in diagnostic testing technologies and their impact on the healthcare industry.
Advancements in Point-of-Care Testing: How Rapid Results are Revolutionizing Diagnosis
Diagnostic testing is a crucial aspect of modern medicine, allowing healthcare professionals to accurately diagnose and treat various diseases and conditions. In recent years, there have been significant advancements in diagnostic testing technologies, particularly in the field of point-of-care testing. This type of testing, which provides rapid results at the patient’s bedside or in a doctor’s office, has revolutionized the way diagnoses are made and treatments are administered.
One of the key innovations in point-of-care testing is the development of portable and handheld devices. These devices are compact, easy to use, and can provide results within minutes. This has greatly improved the efficiency of diagnostic testing, as patients no longer have to wait for hours or even days to receive their results. Instead, they can be diagnosed and treated immediately, leading to better patient outcomes.
Another major advancement in point-of-care testing is the use of biosensors. These are devices that can detect and measure specific biological substances, such as proteins, enzymes, and DNA, in a patient’s sample. Biosensors are highly sensitive and can provide accurate results in a matter of minutes. They are also cost-effective and can be used in a variety of settings, from hospitals to remote areas with limited resources.
One of the most significant benefits of point-of-care testing is its ability to provide rapid results. This is especially crucial in emergency situations, where time is of the essence. For example, in cases of heart attacks or strokes, every minute counts, and a quick diagnosis can mean the difference between life and death. With point-of-care testing, healthcare professionals can quickly determine the cause of a patient’s symptoms and provide appropriate treatment.
Moreover, point-of-care testing has also improved the accuracy of diagnoses. In traditional laboratory testing, samples may need to be transported to a central lab for analysis, which can lead to delays and potential errors. With point-of-care testing, the sample is analyzed immediately, reducing the risk of contamination or sample degradation. This results in more accurate and reliable diagnoses, leading to better treatment plans for patients.
In addition to its use in emergency situations, point-of-care testing has also been instrumental in managing chronic diseases. For patients with conditions such as diabetes, regular monitoring of blood glucose levels is crucial. With point-of-care testing, patients can easily and quickly check their blood sugar levels at home, without the need for frequent visits to a lab or doctor’s office. This not only improves the patient’s quality of life but also allows for better management of their condition.
Another key innovation in point-of-care testing is the integration of digital technology. With the rise of smartphones and other mobile devices, healthcare professionals can now use apps and other digital tools to analyze and interpret test results. This not only makes the process more efficient but also allows for better data management and analysis. It also enables remote monitoring, where patients can share their test results with their healthcare providers in real-time, allowing for timely adjustments to their treatment plans.
Despite its many benefits, point-of-care testing does have some limitations. One of the main challenges is ensuring the accuracy and reliability of results. As with any diagnostic test, there is always a risk of false positives or false negatives. Therefore, it is crucial for healthcare professionals to carefully select and validate the point-of-care testing devices they use.
In conclusion, advancements in point-of-care testing have revolutionized the way diagnoses are made and treatments are administered. The development of portable devices, biosensors, and digital technology has greatly improved the efficiency, accuracy, and accessibility of diagnostic testing. As technology continues to advance, we can expect to see even more innovations in point-of-care testing, leading to better healthcare outcomes for patients worldwide.
The Role of Artificial Intelligence in Diagnostic Testing: Enhancing Accuracy and Efficiency
Diagnostic testing plays a crucial role in the healthcare industry, aiding in the early detection and treatment of diseases. With advancements in technology, diagnostic testing has also evolved, becoming more accurate and efficient. One of the key innovations in diagnostic testing technologies is the integration of artificial intelligence (AI).
AI refers to the simulation of human intelligence processes by machines, including learning, reasoning, and self-correction. In the field of diagnostic testing, AI has been utilized to enhance accuracy and efficiency, ultimately improving patient outcomes.
One of the main advantages of AI in diagnostic testing is its ability to analyze vast amounts of data quickly and accurately. Traditional diagnostic methods often rely on human interpretation, which can be prone to errors and subjectivity. With AI, data can be analyzed in a matter of seconds, reducing the risk of human error and providing more reliable results.
Moreover, AI can continuously learn and adapt, making it a valuable tool in diagnostic testing. As more data is fed into the system, AI algorithms can improve their accuracy and make more precise diagnoses. This is particularly beneficial in complex cases where multiple factors need to be considered.
AI has also been integrated into imaging technologies, such as MRI and CT scans, to aid in the detection of abnormalities. These technologies produce large amounts of data, which can be overwhelming for human interpretation. AI algorithms can analyze this data and highlight any abnormalities, allowing healthcare professionals to focus on the areas of concern.
In addition to accuracy, AI has also improved the efficiency of diagnostic testing. With the ability to analyze data quickly, AI can reduce the time it takes to make a diagnosis. This is especially crucial in emergency situations where time is of the essence. AI can also prioritize urgent cases, ensuring that patients receive timely and appropriate care.
Another key innovation in diagnostic testing is the use of AI-powered chatbots. These chatbots can interact with patients, gathering information about their symptoms and medical history. This data is then analyzed by AI algorithms, providing healthcare professionals with a preliminary diagnosis. This not only saves time but also allows for more efficient use of resources, as patients with less urgent cases can be directed to alternative care options.
Furthermore, AI-powered chatbots can also assist in remote patient monitoring. Patients can input their symptoms and vital signs into the chatbot, which can then alert healthcare professionals if there are any concerning changes. This allows for early detection of potential health issues and can prevent unnecessary hospital visits.
AI has also been utilized in the development of predictive models for disease diagnosis. By analyzing large amounts of data from patient records, AI algorithms can identify patterns and risk factors for certain diseases. This can aid in early detection and prevention of diseases, ultimately improving patient outcomes.
However, the integration of AI in diagnostic testing also presents some challenges. One of the main concerns is the potential for bias in the algorithms. If the data used to train the AI is biased, it can lead to inaccurate diagnoses and perpetuate health disparities. To address this issue, it is crucial to ensure that the data used to train AI algorithms is diverse and representative of the population.
In conclusion, the role of AI in diagnostic testing is rapidly expanding, with the potential to revolutionize the healthcare industry. Its ability to analyze vast amounts of data quickly and accurately, improve efficiency, and aid in early detection and prevention of diseases makes it a valuable tool for healthcare professionals. However, it is essential to address any potential biases and continue to monitor and improve AI algorithms to ensure their effectiveness and ethical use in diagnostic testing.
Next-Generation Sequencing: Unlocking the Potential of Genetic Testing for Disease Diagnosis
Next-generation sequencing (NGS) has revolutionized the field of genetic testing, allowing for faster, more accurate, and more comprehensive analysis of an individual’s genetic makeup. This technology has opened up new possibilities for disease diagnosis, as it can detect a wide range of genetic variations that were previously undetectable. In this article, we will explore the key innovations in NGS and how they are unlocking the potential of genetic testing for disease diagnosis.
One of the major advancements in NGS is the ability to sequence the entire human genome in a matter of days, compared to the years it would take with traditional methods. This is made possible by the development of high-throughput sequencing machines, which can process large amounts of genetic data simultaneously. These machines use a technique called massively parallel sequencing, where millions of DNA fragments are sequenced at the same time, greatly increasing the speed and efficiency of the process.
Another key innovation in NGS is the development of targeted sequencing. This technique allows for the selective sequencing of specific regions of the genome, rather than the entire genome. This is particularly useful for disease diagnosis, as it allows for the identification of specific genetic variations that are known to be associated with certain diseases. Targeted sequencing is also more cost-effective and time-efficient compared to whole-genome sequencing, making it a popular choice for clinical applications.
One of the most significant advantages of NGS is its ability to detect a wide range of genetic variations, including single nucleotide polymorphisms (SNPs), insertions, deletions, and copy number variations (CNVs). SNPs are the most common type of genetic variation, and they can have a significant impact on an individual’s risk for developing certain diseases. By detecting these variations, NGS can provide valuable insights into an individual’s genetic predisposition to diseases such as cancer, cardiovascular disease, and neurological disorders.
In addition to detecting genetic variations, NGS also allows for the identification of rare and novel mutations. These mutations may not be present in large enough numbers to be detected by traditional methods, but they can have a significant impact on an individual’s health. NGS can also detect mutations in non-coding regions of the genome, which were previously considered “junk DNA” but are now known to play a crucial role in gene regulation and disease development.
NGS has also made significant strides in improving the accuracy and reliability of genetic testing. With traditional methods, there was always a risk of human error or contamination, which could lead to incorrect results. NGS, on the other hand, is highly automated and requires minimal human intervention, reducing the risk of errors. Additionally, the high-throughput nature of NGS allows for multiple samples to be processed simultaneously, reducing the chances of contamination.
The advancements in NGS have also led to the development of new bioinformatics tools and software for data analysis. These tools can handle the massive amounts of data generated by NGS and provide accurate and reliable results. They also allow for the integration of data from different sources, such as electronic health records and family history, to provide a more comprehensive analysis of an individual’s genetic profile.
In conclusion, NGS has revolutionized the field of genetic testing and has unlocked the potential for disease diagnosis. Its ability to sequence the entire genome, detect a wide range of genetic variations, and provide accurate and reliable results has made it an invaluable tool in clinical settings. As technology continues to advance, we can expect even more innovations in NGS, further improving our understanding of the genetic basis of diseases and leading to more personalized and effective treatments.
Microfluidic Technology: Miniaturizing Diagnostic Testing for Improved Accessibility and Affordability
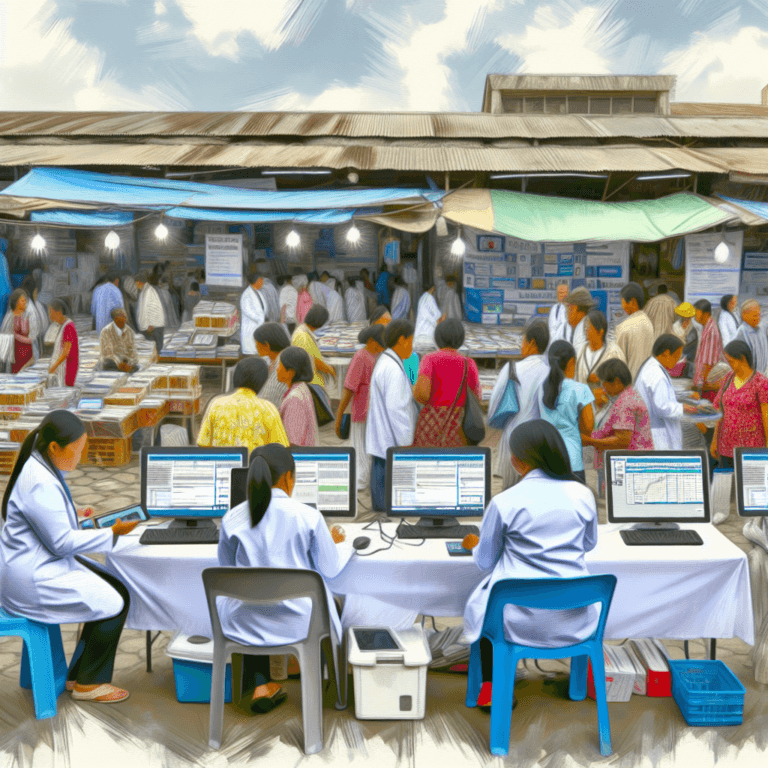
Diagnostic testing plays a crucial role in the healthcare industry, allowing for the early detection and treatment of diseases. However, traditional diagnostic testing methods can be time-consuming, expensive, and require specialized equipment and trained personnel. This can limit accessibility and affordability, especially in developing countries. To address these challenges, microfluidic technology has emerged as a key innovation in diagnostic testing.
Microfluidic technology involves the manipulation of small volumes of fluids, typically in the range of microliters, on a microscale device. These devices, also known as lab-on-a-chip or microfluidic chips, are made up of tiny channels, valves, and pumps that allow for the precise control and analysis of fluids. This technology has revolutionized diagnostic testing by miniaturizing and automating the process, making it more accessible and affordable.
One of the main advantages of microfluidic technology is its ability to reduce the sample and reagent volumes required for testing. Traditional diagnostic tests often require large volumes of samples and reagents, which can be costly and difficult to obtain, especially in remote areas. Microfluidic devices, on the other hand, can perform multiple tests using only a few microliters of sample and reagent. This not only reduces the cost but also makes it easier to collect and transport samples, making diagnostic testing more accessible in resource-limited settings.
Moreover, microfluidic technology allows for the integration of multiple steps in the diagnostic process on a single chip. This eliminates the need for multiple instruments and trained personnel, making the testing process more streamlined and efficient. For example, a microfluidic chip can perform sample preparation, mixing, and analysis all in one device, reducing the turnaround time for test results. This is particularly beneficial in emergency situations where quick and accurate diagnosis is crucial.
Another key innovation in microfluidic technology is the development of point-of-care (POC) diagnostic tests. POC tests are designed to be performed at or near the patient, eliminating the need for samples to be sent to a central laboratory for analysis. This is especially useful in remote or underserved areas where access to healthcare facilities is limited. POC tests using microfluidic technology have been developed for a wide range of diseases, including infectious diseases, cancer, and genetic disorders. These tests are not only faster and more convenient but also reduce the burden on healthcare systems and improve patient outcomes.
In addition to improving accessibility and affordability, microfluidic technology has also enhanced the accuracy and sensitivity of diagnostic testing. The precise control of fluids and the miniaturization of the testing process allow for more accurate and reproducible results. This is particularly important in the early detection of diseases, where even a small deviation in results can have a significant impact on patient outcomes. Microfluidic devices also have the potential to detect diseases at an earlier stage, increasing the chances of successful treatment.
Furthermore, microfluidic technology has enabled the development of personalized medicine, where treatments are tailored to an individual’s genetic makeup. By integrating genetic analysis on a microfluidic chip, healthcare providers can quickly and accurately identify genetic variations that may affect a patient’s response to certain medications. This allows for more targeted and effective treatments, reducing the risk of adverse reactions and improving patient outcomes.
In conclusion, microfluidic technology has revolutionized diagnostic testing by miniaturizing and automating the process, making it more accessible, affordable, and accurate. Its potential for point-of-care testing and personalized medicine has the potential to transform healthcare delivery, especially in resource-limited settings. As this technology continues to advance, we can expect to see even more innovative and impactful applications in the field of diagnostic testing.
Q&A
1. What are some key innovations in diagnostic testing technologies?
Some key innovations in diagnostic testing technologies include the development of rapid and portable testing devices, the use of artificial intelligence and machine learning in data analysis, the integration of molecular and genetic testing, and the advancement of point-of-care testing. These innovations have greatly improved the speed, accuracy, and accessibility of diagnostic testing, leading to earlier and more effective detection and treatment of diseases.
2. How have rapid and portable testing devices impacted the field of diagnostic testing?
Rapid and portable testing devices have greatly improved the efficiency and accessibility of diagnostic testing. These devices allow for quick and accurate testing at the point of care, reducing the need for samples to be sent to a laboratory and decreasing the time it takes to receive results. This has been especially beneficial in remote or underserved areas where access to traditional laboratory testing may be limited.
3. What role does artificial intelligence and machine learning play in diagnostic testing?
Artificial intelligence and machine learning have revolutionized the field of diagnostic testing by improving data analysis and interpretation. These technologies can quickly analyze large amounts of data and identify patterns and trends that may be missed by human analysis. This has led to more accurate and efficient diagnosis of diseases, as well as the development of personalized treatment plans based on a patient’s unique genetic makeup.
4. How has the integration of molecular and genetic testing impacted diagnostic testing?
The integration of molecular and genetic testing has greatly expanded the capabilities of diagnostic testing. These tests can detect specific genetic markers or mutations that may indicate a predisposition to certain diseases or help identify the most effective treatment options. This has led to more targeted and personalized healthcare, as well as improved early detection and prevention of diseases. Additionally, molecular and genetic testing has also allowed for the development of new diagnostic tests for diseases that were previously difficult to detect.
Conclusion
In conclusion, the advancements in diagnostic testing technologies have greatly improved the accuracy, speed, and accessibility of medical diagnoses. From the development of new testing methods such as PCR and ELISA, to the integration of artificial intelligence and machine learning in diagnostic tools, these innovations have revolutionized the field of medicine. They have not only allowed for earlier and more accurate detection of diseases, but also enabled healthcare professionals to make more informed treatment decisions. With ongoing research and development, we can expect to see even more groundbreaking innovations in diagnostic testing technologies in the future, ultimately leading to better patient outcomes and improved overall healthcare.